Chronic and Persistent Pain are associated with a variety of social stigmas. Pain science is showing us that many of these commonly accepted thoughts about how to treat and manage pain are fundamentally flawed and not support by current evidence or our clinical experience. A significant portion of time with patients is spent dispelling some of these thought errors and updating them on what current evidence is showing. Below are some key erroneous thoughts we have found in our time treating many patients who have quickly resolved their chronic pain through our treatment system.
Myth #1: Pain is proportionate to damage
Our previous cultural experience with pain is that pain is meant to signal damage. This is a reasonable assumption from the experience of many of our lives; you hit your knee or smash your thumb and it hurts. Larger injuries, like a broken bone, can hurt more. But there is a significant amount of research and life experience that shows us pain is not a measure of damage. One of my favorite examples to talk about is a paper cut. We have all had a paper cut and all remember the experience as painful. This is even more true if we keep hitting the paper cut throughout the day or get salt or lemon juice on that papercut. By the end of the day, that papercut is throbbing and red. Despite this reality, we would all be hard pressed to name a single person who has been hospitalized due to a papercut. The evidence against pain signaling damage goes well past our anecdotes. A very cold stimulus can be increased or decreased in pain based on whether a red or blue light is shown with the stimulus (red light makes more pain). Studies have compared military and civilian injuries repeatedly, highlighting that many soldiers had reduced or no pain until they were sage. One study showed that “there was no dependable relation between the extent of a pathological wound and the pain experienced” Let’s pause and think about this. These soldiers had obvious extensive wounds, were not in shock, and were mentally clear. Despite the obvious wounds, only 25% of the soldiers wanted to do anything about the wound. Civilians regularly reported more pain and a higher need for narcotics.
Let’s move even further, because we can all realize that war and military conflict creates a unique mental space. Even in the civilian population, there is a large amount of ever-increasing evidence that does not correlate pain to structural damage. Back pain, neck pain, and knee osteoarthritis have all shown a lack of correlation to changes on various imaging (meaning an xray or an MRI). What this means is that the amount of pain has no correlation to actual changes in the human body. This means that pain does not signal changes to the structure in the body. Pain is a much larger conversation of meaning and context in which pain occurs.
Truth: Pain is Proportionate to Meaning
Myth #2: Pain is an inevitability of aging
This is a common point of conversation in our clinic. We frequently catch a patient casually stating that “they are just getting older.” There are actually two common replies to this thought. The most prominent is that there is no evidence suggesting that pain must increase when we age. It simply does not exist anywhere. There is no book, no experiment, or study that states pain increases with age. I can not provide a link for this fact because there is no such evidence. The evidence is actually to the contrary. Pain actually decreases as we age. Several studies show that at least part of the mechanism for this is because our nervous system degenerates.
Part of this belief holds significant bias in our current US culture. Many of our patients have parents with chronic pain and one of their major motivations are avoiding that life for themselves. But this is a small section of humans in a small region on earth in a small time frame. Just because our parents, in the United States, born after 1900, have pain as they age does not fundamentally mean that all older people have pain. Beyond our borders and experience, many cultures and peoples experience pain very differently.
Truth: Aging Does Not Demand More Pain
Myth #3: Rest is good
One of the more perplexing experiences of patients is the notion of rest. So many patients come to us and have real time relief in one treatment only by using our movement system. But these same patients will aggravate something in the weeks or months to follow and then state they then “took it easy for a few days.” I think our treatments greatest value is that we can show patients that they can literally heal themselves. Most relief from most appointments occur before we actually touch our patients at all. Despite this actual experience, our idea of pain still defaults most people to resting. I can fully admit that sometimes an injury warrants rest. In 2015 I low-sided on a scooter and took the entirety of the impact on the right side of my rib cage. I broke several ribs and dislocated several ribs at the sternum. At the time of the accident and for 2 hours after, I literally had no pain. I performed every test I think I could perform and had no pain. Then once I was home and safe the pain really started. It was bad. It was very very bad. Sneezing or coughing was a serious and real crisis usually follow by excruciating pain and audible pops as ribs dislocated and shifted. I absolutely rested with that injury . . . for 1 week. After that I was doing rehabilitation every single day. When I started I could barely do anything, but I did what I could and grew my movement capacity week after week.
Personal experience aside, research overwhelmingly supports movement for the reduction of all pain and particularly chronic pain. To quote Lorimer Moseley, “Motion is Lotion.” Exercise creates a local analgesic pain response in the areas of motion and downregulates pain pathways. Most importantly, it also produces Human Growth Hormone. HGH is the primary hormone responsible for creating repair in the body. The most effective way to increase HGH production to use weight bearing compound movements. This is one of many reasons why we teach all patients to hinge and then expand that system to weighted deadlifts. It is the safest and easiest way to increase HGH for our patients.
Fact: Motion Reduces Pain
Myth #4: Extra Weight Will Increase Joint Pain
For a long time, I was in this camp as well. The logic is sound. Extra weight means more stress on any part of the body. I loosely held this belief until I stumbled across this placard at Bodies: The Exhibition at OMSI.
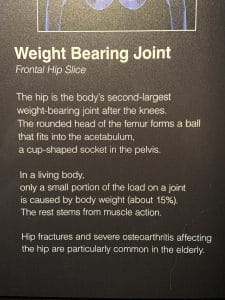
After reading this, I immediately knew that someday I would write about that placard. To highlight the important part:
Only a small portion of the load on a joint is caused by body weight (about 15%). The rest stems from muscle action.
We have reached another stop and think moment. What this means is that the large majority of joint load come from movement and NOT from a bodies weight. Lets do some math to demonstrate how powerful this statement means. Lets take a person who is 250 lbs. Based on the information above this creates 37.5 lbs of load on a joint. They lose 20 lbs of weight, which is a significant amount of weight loss, and now weigh 230 lbs. This reduces the load to on a joint to 34.5 lbs. They only reduced the load on their joints by 3 lbs or by 9%. This is a ridiculously small change for such a huge weight loss number. Now, I must admit that is is very very fuzzy math and likely very different based on many factors, especially which joint we are talking about. Regardless, whatever the accurate math is, it will show that weight loss creates very little change to a joint’s load. What it also shows is that most joint degeneration is a matter of how that joint is used (ie how local musculature interacts with the joint) and not how much you weigh.
Fact: Most Joint Load Comes From Muscle Action, Not Weight
Myth #5: No Pain, No Gain
It took me many years to realize the difference between hard work and straight out damage. Exercising at your limits is, inherently, and unpleasant tasks. Under artificial circumstances the human body has a hard time pushing the envelope. The voluntary act of creating muscular or cardiovascular fatigue has many distinct feelings trying to coerce you into stopping whatever you are doing. The willing act to suffer is where this adage comes from. To achieve great things physically, discomfort is expected. After a few decades of exercise under my belt I now know there is a distinct difference between hard work and hurt. It wasn’t until I had the absence of discomfort that I realized how much damage I had been producing in my body. I can still distinctly remember the first time I deadlifted without any low back strain at all. I put the weight down and thought to myself: “Huh, it just felt like I used only my legs. No wonder people can do crazy amounts of leg work. They are just using their legs.” Ever since that moment I have been able to find in myself, and in our patients’, ways to complete movements just by doing old fashioned hard work and without strain. Christopher Summer, lead coach behind GymnasticsBodies.com, summarized the concept of training versus hurting beautifully. If you are feeling discomfort and stop, muscles will recover quickly and the discomfort should go away within 1 – 2 minutes. If the discomfort doesn’t go away in 2 minutes, you are doing damage. For a large majority of the population, this is the only advice you will ever need to exercise without hurting yourself. This logic, however, can get a little fuzzy in the world of chronic pain.
As I discussed before, chronic pain is mostly unnecessary over protection. Whatever initial trauma created pain has had some sort of resolution and there is likely no significant anatomical problem any more. I would remind anyone that that statement does not mean the pain is not real. The pain is very real, it’s just not accurate of reality. In our chronic pain patients we do see some movements are initially painful and many movements create apprehension, but even these signals go away upon stopping. This apprehension and pain generally go away within 3 treatments (which is incredibly fast in the world of chronic pain). What we fundamentally need to realize is the brain is still inappropriately linking their current reality to a previous painful experience. A common initial injury to persistent low back pain is simply picking up something. It is usual in an awkward position and it is rarely a heavy item. It usually would look something like this:

That is very different in position and load on the low back than how we teach people to pick items up or sit to a chair.
 .
. 
In the presence of chronic low back pain, ANY motion remotely similar to “bending over” will create a pain response, even when those positions are extremely different from each other or a position that many people have not done for decades*. The result will be immediate pain. But this pain will stop upon either stopping the motion or repetition of hinging (or whatever pattern we are fixing). So, again, the idea of training through pain is not accurate when it comes to chronic pain. We always tell patients that the right motion may start with pain but then will eventually reduce pain, usually within 1 treatment.
Fact: Hard Work is Different Than Pain
The frustrating reality of chronic pain is that this is only a small sample of the many myths we have been told or we tell ourselves. We could easily join the throngs of authors and clinicians rewriting the story of what it means to treat pain and how to treat it. Regardless of where you go or who you see, remember that there is extremely promising evidence for changing pain and improving the quality of your life.
*As a special note, all humans who are born without congenital defects have hinged before. It is genetically hardwired in all of us to pick up items with a stable spine and use the large muscles of the hips. Many of us have simply forgot how to do that. In fact, all of our treatment paradigms are genetically hardwired in us. We are simply reminding the body of how to do those acts again.